Sleep Training Deep Dive
A review of the research on sleep training, including whether sleep training improves sleep, whether it causes stress for infants, and whether it has any long-term impacts
Source: Dobromir Dobrev/Pexels
Welcome to the Parenting Translator newsletter! Subscribe here for more research-backed tips for parents!
It often seems that every parent and every parenting “expert” has an opinion on sleep training that involves one extreme or another— either sleep training is essential to helping children learn how to sleep and “self-soothe” or sleep training will irreparably harm your child and is equivalent to child abuse. Even parenting books provide conflicting advice. About two-thirds of parenting books advise parents to use sleep training while one-third of parenting books advise against it. This leaves the average parent feeling, at best, confused and, at worst, shamed for whatever choice they make.
So what does the research actually say? Can diving into the research help us to understand why both sides of the debate claim to be backed by research? This is an extensive, in-depth overview of the research so for the TL;DR skip to the Overall Translation at the end of this newsletter or the Translation at the end of each section.
To listen to this newsletter, check out the podcast here:
Different Sleep Training Methods
Before diving into the research, it is first important to define what “sleep training” might actually mean since nearly every research study uses a different definition. In nearly all of the more recent, high-quality studies, sleep training is not simply “cry-it-out” (aka shutting the door and letting your infant cry until they fall asleep). Sleep training in research often involves more “gentle” and gradual methods because this is what most researchers and experts recommend. Possible sleep training methods are as follows:
Extinction or “Cry-It-Out”: This approach typically involves the parents putting the child to bed awake at a particular time and then leaving the room and ignoring all cries or calling out for the parents until the morning. Most recent research studies do not use this more strict version of sleep training.
Modified Extinction, or “Checking In”: This is one of the most popular sleep training approaches and has many names including the “Ferber method,” “intermittent responding,” and “spaced soothing.” This approach varies across different studies but typically involves the parents putting the child to bed awake and then leaving the room and ignoring any cries or calling out for a specific period of time. The parents then “check in” on the child at a fixed schedule (such as every 5 minutes) or at progressively longer intervals (such as 5 minutes, then 10 minutes, then 15 minutes). The checking in procedure may involve a very brief visit to the child’s room with verbal reassurance, replacing a sleep aid (such as a pacifier or lovey), or helping the child to get into a comfortable sleeping position. Parents continue this procedure until the child falls asleep and then again at any nighttime awakenings.
Parental Presence or “Camping Out”: The “Camping Out” method is similar to the “Checking In” method, except parents remain present throughout the night. The idea behind this approach is that parental presence during sleep training may be less distressing for some infants. In this approach, parents spend the night sleeping next to the crib on a separate bed or mattress. Parents provide brief verbal reassurance, replace sleep aids (such as a pacifier), and help the child get into a comfortable position every few minutes if the child cries or protests. The parent then returns to their own bed. After several days of Camping Out, the parents may gradually remove their presence from the room, first during the nighttime awakenings and then at bedtime.
Bedtime Fading: This procedure involves delaying bedtime until a time that the child will fall asleep quickly and independently. Bedtime is then gradually moved forward to the desired time by moving it 15 to 30 minutes earlier every night. Parents typically do not alter their response to nighttime awakenings. See here for a guide on how to implement it.
Sleep Education or Positive Routines: Some studies that discuss sleep training only involve educating parents and creating some positive routines around sleep such as telling parents what is “normal” for infant and toddler sleep and how to create a consistent bedtime routine. Nearly all of the more recent studies involve teaching parents these positive routines.
Limitations of the Sleep Training Research
Sleep training research is complicated. We can’t just compare families who choose to sleep train with families who do not because these families are different in so many ways, and we wouldn’t know if the sleep training or the other differences were responsible for the study results. Therefore, it is important that research randomly assign parents to sleep train or not sleep train, and fortunately these types of studies (called randomized controlled trials) have been conducted on sleep training. However, for ethical reasons related to “forcing” such an important parenting decision, most studies do not “force” parents to sleep train but rather only provide information on sleep training, and, for ethical reasons, most studies do not “force” the control group to avoid sleep training but simply do not provide information on sleep training. Therefore, not all of the sleep training group is actually sleep training and not all of the control group is not sleep training (one study found that about 64% of parents will use some kind of sleep training even without being advised to do so by a researcher).
In addition, most sleep training interventions also provide parents with additional support such as how to develop a bedtime routine or the opportunity to meet with a professional to develop an individualized sleep program— so it is unclear whether the results are related to this additional support or sleep training itself.
TRANSLATION: When the studies described below find differences, it is possible that they may be related to the additional support that the intervention group received. When these studies find no differences between groups, it is possible that this is because the intervention and control group are actually not that different (since both may be using some form of sleep training).
Does sleep training work (aka does it actually improve your child’s sleep)?
Research broadly finds that sleep training methods improve sleep for infants according to parent report, yet it is unclear whether they actually improve sleep according to objective measures of actual sleep time. A 2006 review study found that 82% of children show clinically significant improvement in sleep with sleep training. However, most of these studies (77%) used parent report measures, which are limited because the infants may still be waking up even if the parents don’t hear them and parent report of infant sleep may be biased particularly after parents have invested time, energy, and emotion into sleep training.
Fortunately, we have a few randomized controlled trials (translation: the highest quality study design) that use objective measures of sleep, called actigraphy (translation: data from monitors that the infants wear that shows whether or not they actually wake up). One randomized controlled trial of sleep training with 6- to 8-month-olds who had a parent-reported “sleep problem” randomly assigned parents to either get instruction on infant sleep or infant safety. The instructions on infant sleep involved a description of the Checking In method (described above) but also other important information such as the importance of having a bedtime routine. Interestingly, the researchers found that, although parents reported that their babies were waking up less frequently, sleep actigraphy found that the babies in the sleep training group were waking up just as often. However, the actigraphy did find that sleep trained babies slept longer for their first period of sleep before waking— yet, on average they only slept 16 minutes longer. After the intervention, 4% of the sleep training group reported their child still had a sleep problem, while 14% of the control group did. The parents that learned sleep training also reported improved mood, sleep quality, and fatigue. This study had some important limitations. Although the intervention group got information about sleep training, it is unclear whether they actually followed these instructions. It is also unclear whether it was the sleep training or learning other important sleep information such as bedtime routines that resulted in slightly longer sleep times. The researchers also did not determine whether any parents in the control group used sleep training or not.
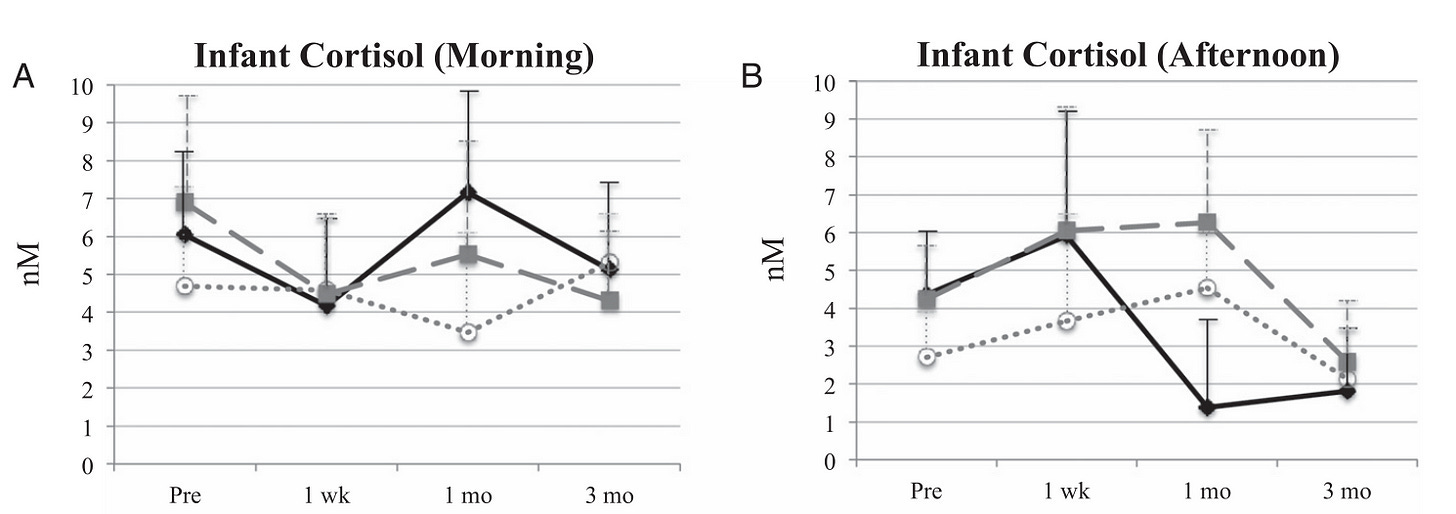
Another randomized controlled trial assigned parents to one of three groups: 1) Checking In, 2) Bedtime Fading, or 3) Sleep Education. The researchers found that both children in the Checking In and Bedtime Fading groups slept better after treatment according to parent report but found no differences according to objective measures of sleep. This may mean that children were not necessarily sleeping better but perhaps were not crying out to parents as often. Although parent report may be biased, it may also be important to look at this data because not crying out to parents may mean that the parents were sleeping better (and sleep deprivation among parents is real so should not be overlooked). Yet, see graphs below that show that, even for parent report, there didn’t seem to be a significant difference in the sleep training group at the end of the intervention for wake after sleep onset (the first stretch of sleep), number of awakenings, or total sleep time. Sleep training also did not result in infants “sleeping through the night.” However, the lack of differences among groups may have been because it is unclear in this study what percentage of parents in the intervention groups actually used the sleep training methods advised by researchers and what percentage of the Sleep Education group might have used sleep training even when they were not advised to do so.
Source: Gradisar, M., Jackson, K., Spurrier, N. J., Gibson, J., Whitham, J., Williams, A. S., ... & Kennaway, D. J. (2016). Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics, 137(6).
A question commonly asked with sleep training methods is whether they lead to any long-lasting changes. One randomized controlled trial followed children for 5 years and focused only on 8- to 10-month-olds with reported “sleep problems.” They allowed mothers to choose either the Checking In or Camping Out method and taught parents how to use the strategy of their choice as well as positive sleep strategies, such as bedtime routines. The control group also included consultation with a nurse about their infant’s sleep (although the nurse wasn’t specifically trained in these techniques, she may still have recommended sleep training). The first report of this study found that mothers were less likely to report their child still had a sleep problem by 10 and 12 months. Yet, 56% of mothers at 10 months and 39% of mothers at 12 months still reported a sleep problem even after sleep training (versus 68% of the control group at 10 months and 55% at 12 months). A follow-up study found that the difference between the intervention and control group faded by age two. At 2 years, researchers found that 27% of the intervention group versus 33% of the control group still reported their child had a sleep problem (this difference was not significant). Another follow-up study also found no difference in whether parents reported sleep problems at 3 or 4 years. In the final follow-up study at 6 years, the researchers found no difference in sleep between the two groups, including whether parents reported sleep problems or differences in children’s sleep habits. These findings suggest that the benefits of sleep training may be temporary and not necessary for a child to develop independent sleep skills.
TRANSLATION: Sleep training may result in modest, temporary improvements in at least parent-reported sleep for children over 6 months yet it does not seem to be a “silver bullet” that reduces all sleep problems and always results in “sleeping through the night.” Sleep training is also unlikely to result in long-term improvements in sleep (translation: sleep training an infant does not mean your child is guaranteed to be a “good sleeper” as a toddler or preschooler or vice versa, that not sleep training an infant means they will be a “poor sleeper” as a toddler or preschooler). Two randomized controlled trials suggest that sleep training increases the first stretch of sleep by about 15 minutes when compared to a control group (one found this with actigraphy and one only with parent report). Some sleep-deprived parents may conclude from this data that parent-reported improvements in sleep and the possibility of 15 minutes of extra sleep for their baby is very significant to their quality of life and decide to attempt sleep training. However, other parents may conclude from this data that sleep training may not be worth it without consistent evidence for objective and long-lasting improvements in sleep. This research also indicates that you do not need to sleep train to improve your infant’s sleep or that if you do not sleep train your child will never get adequate sleep and/or learn independent sleep skills. In summary, it is really up to you as a parent whether it is worth it to sleep train.
What about sleep training for babies 6 months and younger?
It is very important to mention that we do not have sufficient evidence that sleep training is effective before 6 months. One of the only randomized trials of young infants found no impact of educating parents about infant sleep before 12 weeks, including tips such as allowing the baby to fall asleep independently without feeding or rocking them to sleep. Another larger randomized controlled trial of educating parents about infant sleep before 6 months that included both tips like putting the baby to sleep independently without feeding or rocking them and information on the Checking In method found no differences in parent-reported sleep problems and objective measures of sleep found that the intervention only decreased night awakening by 8% and that the babies only slept for 6 minutes longer during the day.
TRANSLATION: We do not have any evidence that any type of sleep intervention (including more gentle methods) will significantly improve the sleep of infants under 6 months. In the first six months, do whatever works best for you and your baby and do not worry about forming “bad habits”!
Does sleep training cause stress for infants?
One of the biggest hesitations that parents have about sleep training is that it might cause undue stress for their infants. So does it really cause stress?
One study of the Checking In and Bedtime Fading methods looked at morning and afternoon cortisol in infants (translation: cortisol is a hormone that normally increases during stress). The researchers found no differences in morning cortisol and found that the Checking In group showed a larger reduction in afternoon cortisol than the Bedtime Fading or Sleep Education groups at 12 months after the intervention. However, there was an initial increase in afternoon cortisol in the sleep training groups (see graph below) and there were no differences among groups at 3 months after the intervention. However, it is hard to know how to interpret these results since the researchers did not measure cortisol during the actual sleep training but rather only in the morning and afternoon one week after the sleep training. Previous research in infants suggests that a peak in cortisol is likely to happen more immediately after a stressful event rather than a week later. This study also had a very small sample size (less than 15 infants per group).
Source: Gradisar, M., Jackson, K., Spurrier, N. J., Gibson, J., Whitham, J., Williams, A. S., ... & Kennaway, D. J. (2016). Behavioral interventions for infant sleep problems: a randomized controlled trial. Pediatrics, 137(6).
A larger follow-up study also found no differences in cortisol levels for children in the sleep training group (Checking In or Camping Out in this study) versus the control group five years after sleep training. Yet, this finding isn’t really that helpful because again they did not test cortisol immediately after the stressful event but five years later.
Another very small study measured cortisol levels during sleep training. This study involved unmodified extinction (strict Cry-It-Out) in a hospital setting. Nurses and mothers would prepare the infant for sleep and then nurses would put the infant to sleep in a crib in a room separate from their mothers. Nurses were then responsible for the infants’ nighttime care while mothers were responsible for daytime care. They measured cortisol at the beginning of the bedtime routine and then 20 minutes after falling asleep on the first and third day of sleep training. The researchers found no differences in cortisol before or after the sleep training. However, for mothers there was a decrease in cortisol from before to after the sleep training. This means that after sleep training the infants’ cortisol levels were not synced up with their mothers. The authors argue that, when the infants and mothers’ cortisol levels are not synced up, it may mean the mothers become less responsive to the infant, which may ultimately weaken the parent-child attachment. However, this study had several important limitations. First and most importantly, they did not have a control group to look at the impact of a nurse putting an infant to bed in a hospital setting without sleep training. It makes sense that this situation in itself would be more stressful for infants than their mothers. The researchers also only measured cortisol for three days and it is possible that the infants’ cortisol levels would have synced back with the mothers.The mothers also got a few “nights off” of caregiving responsibilities and improved sleep (a situation which likely would have reduced cortisol).
TRANSLATION: We do not know whether sleep training is stressful or not for infants based on the research we have. Many different factors may impact an infant’s cortisol and we need further research before concluding that sleep training has a negative impact or a negligible impact on infants’ cortisol.
Does sleep training have long-term negative impacts?
One small study (described above) randomly assigned parents to Checking In, Bedtime Fading, or a Sleep Education control group. The researchers then assessed the children’s attachment one year later and found no difference between groups in parent-child attachment (secure versus insecure attachment). They also found no difference in child emotional or behavioral problems one year later. Yet, this study had very small sample sizes (less than 15 children per group). In addition, it is unclear how different the sleep training groups were from the control group in practice. The control group (the Sleep Education group) was also advised to put the infant in bed awake which may have resulted in sleep training.
Another study with larger sample sizes randomly assigned parents to sleep training (either the Checking In or Camping Out method) or a control group which also had consultations with a nurse (just not a nurse who had been specifically trained in these procedures). The researchers found that the sleep training group did not show any differences in child mental health or parenting practices at 2 years when compared to the control group. When researchers followed up with this group at 3 to 4 years, they found no difference in child behavior or family functioning between groups. At the 6 year follow-up, the researchers found no differences in any measure of child mental health or any measure of the child-parent relationship (including child emotional or behavioral problems, child-parent closeness, quality of life, child stress, and parenting styles). However, as discussed above, it is unclear the extent to which the sleep training group actually engaged in sleep training and the extent to which the control group did not. The researchers reported that many of the families in the intervention group opted out of “Checking In” sleep intervention and instead chose Bedtime Fading or other methods such as creating a bedtime routine or opted out of meeting with a nurse entirely. The control group also had a sleep consultation with a nurse who was not specifically trained in these sleep techniques but could still have recommended similar strategies. In addition, the researchers found that the control was significantly more likely than the intervention group to seek professional help (such as from their pediatrician or a sleep consultant) who may have recommended sleep training. Therefore, if the sleep training group and control group were not different in practice, it makes sense that researchers would find no differences in outcome measures.
TRANSLATION: The research we have so far provides no evidence for long-term harms from sleep training. However, these studies all have serious limitations that make it difficult to assume that these results are conclusive. Some parents may look at this research and decide that they need more evidence from higher-quality studies before concluding that sleep training has no negative outcomes. Some parents may look at this research and feel comfortable choosing sleep training for their family, particularly when sleep deprivation is having a negative impact on family functioning.
Does sleep training improve parent mental health?
In the debate around sleep training, it is also critically important that we consider a parent's mental health. One study that instructed parents to use either the Checking In or Camping Out found that the intervention resulted in slightly lower levels of depression in mothers, with 28% of the mothers in the sleep training group and 35% of mothers in the control group reporting clinically significant depression. At the 2-year-follow up for this study, researchers found that mothers were less likely to report symptoms of depression if they were in the sleep training group (15% vs 26%). However, this intervention group also received more individualized support, including advice related to self-care, and education about infant and toddler sleep more generally, which may have improved the parents’ mental health rather than the sleep training itself. When researchers followed up with children five years later, they found no difference in any measure of parent mental health outcomes or of child-parent relationship (including maternal depression, anxiety, or stress).
TRANSLATION: Sleep training may reduce symptoms of maternal depression, at least in the short-term. However, it is unclear whether it is the sleep training itself or the individualized support provided as part of the sleep training intervention that improves mental health. Providing parents with any type of plan for addressing their child’s sleep likely improves parent self-efficacy (translation: believing you are capable of successfully resolving your child’s sleep issues in this case) and research finds that increasing self-efficacy likely improves parent mental health. This research suggests that simply coming up with a plan to address your child’s sleep problems may benefit mental health.
Is sleep training the only option for improving sleep?
Many parents don’t feel comfortable with a sleep training option that might involve a lot of crying so it is important to know that research finds several other approaches that you can try instead (or try before attempting sleep training).
Implement a consistent, predictable bedtime routine with calming activities: As explained above, most of the studies on sleep training also included sleep education in addition to sleep training and the positive results on infant sleep and parent mental health may be related to this general education rather than sleep training specifically. One strategy that is consistently backed by research is having a consistent and calming bedtime routine. A large randomized controlled trial of infants and toddlers 7 to 36 months found that randomly assigning parents to a bedtime routine resulted in fewer nighttime awakenings and children falling asleep more quickly. Another study found that implementing a bedtime routine resulted in improved sleep in as few as three nights. Given the benefits of a bedtime routine and the lack of risks associated with a bedtime routine, this research suggests that a consistent and predictable bedtime routine should be part of every baby and child’s bedtime.
Seek help from others: When parents were asked about the strategies of a sleep intervention that they found the most helpful, they reported that it was most helpful just having someone to talk to. If you are struggling with your child’s sleep then just having someone to talk to about it may be more helpful than any intervention. This could be your pediatrician, a sleep consultant, or simply a trusted friend.
Do nothing and wait for it to get better: It is important to remember that not sleeping through the night is normal for infants and even young toddlers and you do not have to do something about it if you don’t want to. Research finds that, at 6 months, 57% of mothers reported that their infants were NOT sleeping through the night (8 consecutive hours). At 12 months, 43% of mothers reported that their infants were not sleeping through the night. The researchers also found no association between sleeping through the night and any measure of development or maternal mood.
Try bedtime fading: Bedtime fading simply involves delaying bedtime until a time that the child will fall asleep quickly and independently (and then gradually moving bedtime up to a more optimal time). Research finds that this approach may be associated with improved sleep and may be easier for parents to implement.
Try a more responsive method: A small study of a new more responsive method for sleep training suggested that it may reduce the number of night awakenings (but not increase total sleep duration). More research is needed but this approach involves parents putting the baby down in their crib awake and then patting or stroking them until they fall asleep. After a few nights of this, parents then only use verbal reassurance to help soothe the baby to sleep. The parents then gradually move closer to the door every night and can eventually leave the room for short periods of time while providing verbal reassurance.
I feel comfortable with sleep training, so which method should I choose?
What if you are comfortable with sleep training and ready to get started— how do you choose which method to use? The research studies described above each involve parents using different methods for sleep training and it is unclear the extent to which parents followed the researchers’ instructions for sleep training. Therefore, contrary to what books and sleep trainers may lead you to believe there is no specific “formula” for successful sleep training that is backed by research.
In addition, nearly every parent who has had more than one child will acknowledge that different methods may work for different children, yet most research studies do not examine how to predict which children will respond best to different methods of sleep training. However, a recent study may provide some insight. In this study, researchers randomly assigned parents of 9- to 18-month-olds with reported sleep problems to use either the Checking In or Camping Out approach. Infants with low levels of separation anxiety seemed to benefit from both interventions, showing longer sleep periods following both interventions. However, for infants with higher levels of separation anxiety, only the Camping Out method seemed to improve their sleep. In other words, for children with higher levels of separation anxiety, the Camping Out method seemed to be more effective.
Another study (described in greater detail above) directly compared the Checking In and Bedtime Fading programs and did not find any significant differences at the end of the intervention in either parent report or actigraphy (objective measures of sleep).
TRANSLATION: The research does not clearly point to one sleep training approach being superior to another. Until we have more research, feel free to use the method that feels right to you.
Overall Translation
In summary, the research on sleep training is limited due to ethical issues, but we currently have evidence that it may result in some temporary improvements in at least parent-reported sleep. However, sleep training does not seem to be a “silver bullet” that cures all sleep problems, and we do not yet have strong evidence that sleep training results in long-lasting improvements in sleep. Therefore, sleep training may be helpful but it also may not be necessary. We have no evidence that you need to sleep train to have a good sleeper or that it helps children to learn to “self soothe.” In other words, parents should feel free to make whatever choice that they feel is best for their children and their family.
The research we have thus far also finds no impact of sleep training on any measure of child development, child mental health, parenting, or the parent-child relationship. There are some methodological issues with these findings that might cause some parents to feel hesitant, while other parents may feel comfortable pushing forward. The decision to sleep train or not is based on a lot of factors that are no one’s business but your own, including how your family functions and your own mental health and sleep needs as a parent, so there is no “right” or “wrong” answer.
There is similarly no “right” way or “wrong” way to sleep train since we have no strong evidence that a particular approach works better than others. Because most studies combine different methods and also include basic sleep strategies (such as a bedtime routine), it is unclear which method is ideal and whether different methods may be more or less effective for different children. If you do not feel comfortable with sleep training, there are a lot of more “gentle” and gradual methods you can try first (such as implementing a consistent and predictable bedtime routine). Some methods may work for some children and not for others. Have confidence that you know your individual child best (that you are the expert on your child) and choose what is best for your child and for your family.
Expert Reviewer
All Parenting Translator newsletters are reviewed by experts to make sure that they are as helpful and as accurate for parents as possible. Given the heated nature of this topic, I sought two expert reviewers for this topic— one a pediatrician and another an expert on child development. I sought reviewers who I thought would be on different “sides” of this argument to make this review as balanced as possible.
Dr. Florencia Segura is board-certified pediatrician and fellow of the American Academy of Pediatrics. Dr. Segura has a practice in Northern Virginia and has been recognized as a “Top Doctor” by Washingtonian magazine. For more information on her and the evidence-based information on pediatrics that she shares, check out her Instagram.
Dr. Kristyn Sommer has a PhD in Developmental Psychology. Dr. Sommer is a researcher at Griffith University. Outside of the university, Dr. Sommer communicates science on social media on TikTok and Instagram.
Wondering how you can support Parenting Translator’s mission and/or express your gratitude for this service? It’s easy! All you have to do is share my newsletter with your friends and/or on your social media!
Thanks for reading the Parenting Translator newsletter! Subscribe for free to receive future newsletters and support my work.
Also please let me know any feedback you have or ideas for future newsletters!
Welcome to the Parenting Translator newsletter! I am Dr. Cara Goodwin, a licensed psychologist with a PhD in child psychology and mother to three children (currently an almost 3-year-old, 5-year-old, and 7-year-old). I specialize in taking all of the research that is out there related to parenting and child development and turning it into information that is accurate, relevant, and useful for parents! I recently turned these efforts into a non-profit organization since I believe that all parents deserve access to unbiased and free information. This means that I am only here to help YOU as a parent so please send along any feedback, topic suggestions, or questions that you have! You can also find me on Instagram @parentingtranslator, on TikTok @parentingtranslator, and my website (www.parentingtranslator.com).
DISCLAIMER: The information posted by Dr. Cara D. Goodwin, PhD, Parenting Translator, and its representatives on the Instagram account @parentingtranslator, TikTok account @parentingtranslator, website (ParentingTranslator.com), and newsletter (parentingtranslator.substack.com), or any other medium or social media platform (the “Information”) is for educational purposes only and is not intended or implied to be a substitute for professional medical, mental health, legal, or other advice. Parenting Translator is not engaged in rendering diagnosis, treatment, counseling, or therapy services by providing the Information, and your use of the Information does not create any practitioner-patient or other treatment relationship between you and Dr. Cara D. Goodwin, PhD, Parenting Translator, or any of its representatives. Dr. Cara D. Goodwin, PhD, Parenting Translator, and its representatives assume no responsibility and expressly disclaim liability for any consequence relating directly or indirectly to any action or inaction you take based on the Information. Reliance on any Information provided by Parenting Translator, its representatives, and contributors, is solely at your own risk. Always seek the advice of your own licensed and qualified medical, mental health, legal, or other professional, and do not disregard professional advice or delay in seeking it based on the Information. Call your medical or mental health professional, or 911, for all emergencies.






You are exactly right that there is no magic solution to sleep. Maybe I should have used that as the title. Even if something works for awhile, it may not work long term
Thank you for this! I learned so much, and I feel like this provided an amazingly thorough overview of the literature and its implications and limitations. I was so surprised to read that sleep training may not "stick" or continue to improve sleep as kids age. In some ways it's disheartening, that there is no magic method to permanently improve sleep, but I can also imagine that it's very reassuring for parents who didn't or don't want to sleep train, to know that if their toddler is a bad sleeper, it's not necessarily because they did something wrong when helping their baby sleep, in the method that was best for them at the time!